Therapy for CKD
Treatment of chronic kidney disease (CKD) varies according to the severity of the disease. However, steps can be taken in all cases to: control hypertension, correct salt and water imbalance, treat urinary tract infections, and reduce risk of heart and blood vessel diseases. You can further slow down progression by lifestyle changes (including an adapted nutrition) additional to regular check ups and medication intake.
Personalised treatment options for CKD include conservative therapy and
renal replacement therapy like dialysis or kidney transplantation.
Conservative treatment in the
CKD pre-dialysis phase
A comprehensive conservative treatment of chronic kidney disease (CKD) uses dietary interventions and medications from earlier stages of the disease until start of dialysis.
Dietary interventions, in particular the reduction of protein intake (low/very low protein diet) is an important part of conservative CKD treatment.
Depending on a more severe level of protein reduction, a supplementation with keto-analogues might be indicated. Clinical studies have shown that this combination may postpone the start of dialysis.
The role of proteins in CKD
Proteins are important for various functions in your body including build-up of muscles and cells for the immune system. Eating the right amount of protein is therefore especially important for CKD patients. Over-consumption of protein, when your kidneys are weak, will lead to a accumulation of nitrogen-containing waste in your body. This can have harmful consequences such as: nausea, weakness, tiredness, shortness of breath and reduced appetite.
- Slow down the progression of the disease
- Prevent the development of secondary diseases
Supported Changeover
In this little video you can learn more on why it is important to reduce your protein intake.
Keto-analogues supplemented reduced protein diet
Keto-analogues supplementation to your reduced protein diet increases the quality of the protein intake. They are nitrogen-free precursors of essential amino acids. Keto-analogues are converted to the respective amino acids in the body. In this way, no additional nitrogen intake occurs and the formation of nitrogen-containing waste products is reduced.
It is important to mention that keto-analogues do not work on their own, they are essential supplements to a protein reduced diet.
Benefits of keto-analogue supplementation
Early treatment of advanced CKD patients with keto-analogue may delay the start of dialysis. Keto-analogue supplementation is a safe and effective way for patients on a protein reduced diet to ensure a sufficient daily intake of essential amino acids.

Please find here a short and comprehensive summary of information to better understand and manage your disease.
Nutrition for you
Find out more about nutrition in CKD, when you are not on dialysis
Renal replacement therapy (RRT)
In CKD stage 5, most patients need a renal replacement therapy, such as dialysis or kidney transplantation.
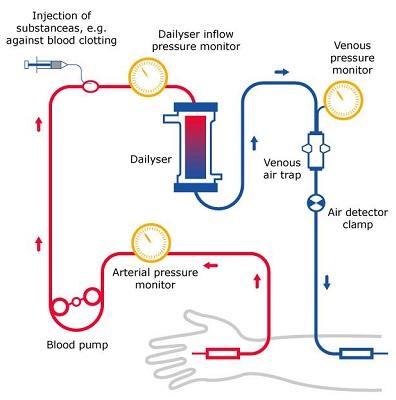
Haemodialysis
Haemodialysis cleans and filters your blood by using a machine to remove harmful wastes, excess salt, and water.
Haemodialysis helps to control blood pressure and helps your body to keep the proper balance of important chemicals such as potassium, sodium, calcium and bicarbonate.1
Inside the haemodialysis machine there is a special filter called a dialyser. The dialyser functions as an artificial kidney. During treatment, your blood travels through a set of tubes into the dialyser that selectively filters out wastes and extra water, but not substances the body needs.
Then, the cleaned blood flows through another set of tubes back into your body. The dialyser is connected to a machine that monitors blood flow and the amount of wastes in the blood as well as the amount of certain substances in the blood and in the haemodialysis fluid.2
To ensure sufficient cleaning of the blood, high blood flow is required. To reach the blood, a so called access is necessary, which is placed by a minor surgery. It is one of the following options:
-
A fistula, an access made by joining an artery and vein in your arm.
-
A graft, an access made by using a piece of soft tube to join an artery and vein in your arm.
-
A catheter, a soft tube that is placed in a large vein, usually in your neck.3
---------------------------------
Sources
1 National Kidney Foundation www.kidney.org/atoz/content/dialysisinfo
(Accessed 03.12.2020)
2 https://www.nhs.uk/conditions/dialysis/what-happens/
(Accessed 04.01.2021)
3 National Kidney Foundation www.kidney.org/atoz/content/hemoaccess
(Accessed 03.12.2020)
4 https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis
(Accessed 04.01.2021)
Each haemodialysis treatment session usually lasts around 4 hours.2
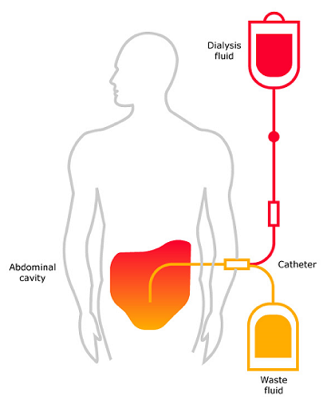
Peritoneal dialysis
This type of dialysis uses the peritoneum inside your abdomen as a filter membrane ("dialyser"). The peritoneum is a thin lining (membrane) that covers the inner wall of the abdominal cavity as well as most of your abdominal organs.
The peritoneal membrane contains many tiny blood vessels and has a large adjoining surface to the abdominal cavity. Therefore, it is appropriate to filter your blood, when your abdominal cavity is filled with a clean dialysis fluid.1
The dialysis fluid is put into your abdomen through a small soft tube. This solution contains a mixture of minerals and sugar dissolved in water. The sugar, called dextrose, draws wastes, chemicals and extra water from the blood vessels in your peritoneal membrane into the dialysis solution.
Types of peritoneal dialysis2
There are two main types of peritoneal dialysis: the Continuous Ambulatory Peritoneal Dialysis (CAPD), typically done during the day and the Continuous Cycling Peritoneal Dialysis (CCPD) that can be performed at night by using a machine that drains and refills the abdomen automatically. Both types of peritoneal dialysis are usually performed by the patient himself after being trained properly.2
If you want to learn more about those therapy options, take a look at this website of Fresenius Medical Care.
---------------------------------
Sources
1 https://nephcure.org/peritoneal-dialysis/ (Accessed 04.01.2021)
2 https://www.nhs.uk/conditions/dialysis/what-happens/ (Accessed 04.01.2021)
3 https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/peritoneal
-dialysis (Accessed 04.01.2021)
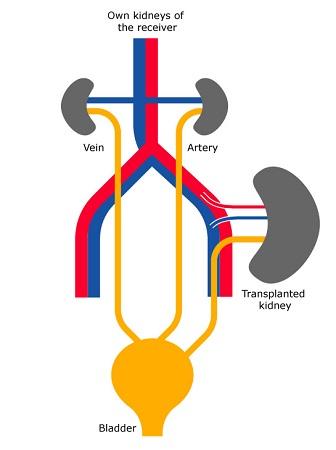
Kidney transplantation1
A kidney transplant procedure places a healthy kidney from another person (donor) into your body. The donated kidney replaces the work that your two failed kidneys used to do.
A successful transplantation returns renal function to nearly normal and frees the patient from dialysis treatment. However, it is not a perfect cure. You have to take a lifelong medication and you have to see your doctor regularly.
How the operation is done
A surgeon places the new kidney inside your lower abdomen and connects the artery and vein of the new kidney to your artery and vein. Your blood flows through the donated kidney, which creates urine, just like your own kidneys did when they were healthy. The new kidney may start working right away or may take up to a few weeks after kidney transplant surgery to produce urine. Unless your own kidneys are causing infection or high blood pressure, they are left in place.
How to find a kidney for transplantation
You may receive a kidney (recipient) from a member of your family (living, related donor), from a person who has recently died (deceased donor) or sometimes from a spouse or a very close friend (living, unrelated donor).1
If you don't have a living donor, you're placed on a waiting list for a deceased donor kidney. The time of waiting for a deceased donor kidney can be several years.
---------------------------------
Sources
1 National Kidney Foundation https://www.kidney.org/atoz/content/kidney-transplant
(Accessed 18.12.2020)
2 https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/kidney-
transplant (Accessed 04.01.2021)